(Note: On Tuesday, Swedish researchers published an article in the European Heart Journal reporting that Vasaloppet competitors are at an increased risk of heart arrhythmias. Their results were striking, and grabbed headlines from science and medicine websites to magazines like The Atlantic and Forbes. In their paper, Dr. Kasper Andersen and his colleagues reported that skiers who competed in more races were at a higher chance of an arrhythmia, with those completing five Vasaloppets having a 30% higher risk, and also that those skiing fastest were at a similarly higher risk. The most common type of arrhythmia was atrial fibrillation.
Arrhythmia has been in the ski news earlier this year, when Norwegian star Marit Bjørgen skipped the Tour de Ski after being hospitalized for one. But what do all these terms mean, and how can you tell if you are at risk? When Andersen’s study was first publicized almost two years ago, we delved into the science and medicine behind the headlines. We’ve updated the piece to include a more detailed breakdown of the risks in the final published paper, which were not available in initial press releases.)
All the way back in 1889, skiing was what originally inspired doctors to examine how sports affect the human heart.
“Skiing causes an enlargement of the heart, and this enlarged heart can perform more work than the normal heart,” wrote a Dr. Henschen. “There is therefore, a physiologic enlargement of the heart, due to athletic activity.’’
Today, skiers are still being used to investigate how endurance training can change the heart. A recent study by Swedish researchers found that elite nordic skiers frequently developed heart arrhythmias. While most people assume that endurance training has only positive effects on cardiovascular health, a growing body of work suggests that a lifetime of exercise can contribute to cardiac abnormalities.
“Basically, this study shows, that even though physical activity is generally healthy, athletes committed to endurance sports at elite level have higher risk of suffering from a heart rhythm disorder,” lead researcher Kasper Andersen of Uppsala University said in a press release. “There seems to be a relation with the duration of the sport commitment and at which level the athletes competed.”
The study surveyed skiers who completed Sweden’s Vasaloppet, one of the longest and most popular races in the world. In all, over 47,000 skiers who competed between 1989 and 1998 were included, and those who had competed five or more of the races had a 29 percent higher frequency of heart arrhythmias.
But Dr. Andresen said that the increase in arrthymias did not lead to an increase in fatalities. So what does this mean for athletes?
The Anatomy of Arrhythmia
Several kinds of irregular heartbeats are included in the loose grouping of arrhythmia. A heart can beat too quickly or too slowly, it can beat too early, or it can simply beat erratically. There are different specific causes of arrhythmia, but all of them are at the most basic level problems with either the structure of the heart or the electrical impulses which cause the heart muscle to contract.
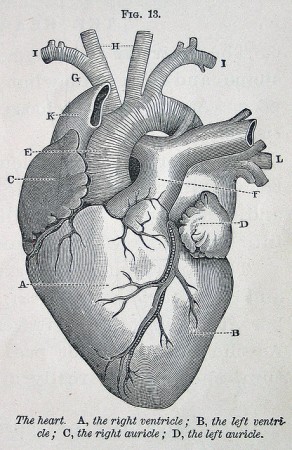
For those who don’t remember high school biology, here’s a basic refresher on the heart. In humans, the heart has four chambers and two different pumping circuits, a low-pressure one to the lungs and a higher-pressure one to the body. Low-oxygen blood returning from the body is pumped through veins into the right atrium, into the right ventricle, and then to the lungs, where it picks up oxygen. The refreshed blood is then sent into left atrium, the left ventricle, and back into the body through the arteries.
All of this movement is caused by powerful muscle contractions, which must be perfectly timed in the different parts of the heart. The atria contract at the same time, about a tenth of a second before the ventricles, and this pattern explains the characteristic “bump-bump” heard through a stethoscope.
The electrical signals which cause the muscle contractions come from pacemaker cells, which are located in the right atrium. The electrical stimuli can pass directly from cell to cell in the heart, meaning that all of the muscles can contract in unison. Once the muscles in the atria contract, the signal passes through a node which controls the pause before the ventricles contract.
How can this process go wrong? Sometimes, instead of producing one strong electrical pulse, the heart produces many weak ones, leading to a fibrillation or a flutter. Other times, the structure of the heart itself may change, for example due to coronary heart disease or vascular disease. Another possible cause is that the electrical circuits may have changed or grown; sometimes additional cells outside the ventricles produce electrical impulses.
In the Swedish study, the most common arrhythmias found in skiers were the erratic and usual heartbeat in the right atria, called atrial fibrillation, and the slow heartbeat, called bradycardia.
What’s So Bad About Bradycardia?
The Vasaloppet paper reported that skiers completing five or more Vasaloppets had a more than twofold increase in risk of a bradycardia compared to skiers that had only done the race once. Bradycardia is defined as a hearbeat under 60 beats per minute, which doesn’t actually get at the underlying causes of the syndrome. For endurance athletes, definitions such as these aren’t particularly useful because having a heart rate under 60 beats per minute is not unusual.
“What’s too slow for you may depend on your age and physical condition,” the American Heart Association writes on its website. “Physically active adults often have a resting heart rate slower than 60 BPM but it doesn’t cause problems.”
Bradycardia is one symptom of the condition known as “athlete’s heart”, in which the resting pulse slows, the left ventricle enlarges, and the heart walls become thicker. These changes are due to regular aerobic exercise; the large muscles in the body require more oxygen to contract and as a result more blood must be pumped in each beat of the heart.
Dr. Paul Thompson of the Hartford Hospital noted in a 2002 paper that bradycardia has been shown to occur in a staggering 91% of endurance athletes. But athlete’s heart isn’t known to have any dangerous side effects, and once athletes stop training, their heart eventually returns to normal. So if bradycardia is simply caused by physiological adaptation to exercise, it probably isn’t a problem.
Another potential cause of bradycardia is what is called atrioventricular block, when the electrical signal from the atria are not fully transmitted to the ventricles. First-degree block is when the electrical impulses are simply transmitted more slowly to the ventricles, causing a delay in the pumping action. In second-degree block, not all of the signals actually reach the ventricles, and in third-degree block, none of the electrical impulses reach the ventricles. Most of the bradycardias reported in Vasaloppet participants were second- or third-degree blocks.
A widely cited 1982 study by Finnish researchers using elite skiers and runners as test subjects found that endurance athletes were more than twice as likely to show first-degree heart block and more than four times as likely to show second-degree heart block compared to the controls. In some cases, the atrioventricular block lasted more than an hour, but the symptoms always disappeared as the heart rate increased during exercise.
The Finnish team did not find believe that these cases of atrioventricular block were particularly dangerous, but they did note that in a small number of cases second-degree heart block can develop into full-blown heart block, which is fatal.
All in all, a review paper in the New England Journal of Medicine noted that athletes shouldn’t be alarmed by bardycardia or first-degree heart block.
“Trained athletes are particularly prone to bradycardia, with heart rates below 40 beats per minute common at rest,” wrote Dr. Michael Mangrum and Dr. John DiMarco. “In one series, sinus pauses lasting between two and three seconds were found in 37 percent of athletes during sleep.”
However, there are some more sinister causes of bradycardia, such as heart disease, low thyroid levels, or electrolyte imbalances. In terms of effects, the danger of the condition is that the body does not receive enough oxygen because blood is moving so slowly and getting refreshed at a lower rate. If a skier has a low resting heart rate and experiences fainting, dizziness, chest pain, low blood pressure, shortness of breath, confusion or trouble focusing, then bradycardia could be the underlying cause and ought to be examined more closely.
All Aflutter About Atrial Fibrillation
For another type of arrhythmia, the researchers found that Vasaloppet participants showed an increased risk of atrial fibrillation of about 9% for each race completed. And the Swedish study isn’t the first to allege that atrial fibrillation (AF) is more common among endurance athletes. A 1997 paper by Finnish researchers showed that elite orienteers were more than five times more likely than the sedentary population to experience AF.
Interestingly, study after study has shown that male athletes are more inclined towards AF than women. AF also frequently appears for the first time in resting situations rather than during exercise.
Unlike bradycardia, the prevalence of AF isn’t simply an issue of definition. There’s no way around the fact that the syndrome is caused by abnormalities in electrical signaling, which is never a positive development. While not always life-threatening, AF can lead to palpitations, chest pain, fainting, stroke, and congestive heart failure.
Most AF cases in athletes are what is called lone atrial fibrillation, which means that there are no accompanying heart defects. While AF is often caused by heart attacks, abnormal heart valves, congenital heart defects, or sleep apnea, in lone AF no other disease is present. Lone AF is caused by electrical disorders rather than structural ones, and it’s rare to have serious complications from lone AF.
Researchers aren’t sure exactly why athletes have a higher prevalence of AF, but inflammation caused by training might be one cause. Inflammation leads an increase in the production of C-reactive protein (CRP), which is positively associated with AF, although why is unclear. Scientists have also hypothesized that the enlargement of the heart chambers might have some effect on electrical signaling.
New Zealand rower Nicola Coles woke up from a nap several weeks before the Beijing Olympics with AF, which persisted for more than 24 hours. After going to the hospital, doctors found that the only way to return her heartbeat to normal was cardioversion, a procedure using electricity and drugs to convert the heart rate.
Coles didn’t experience AF again and went on to place fifth in the women’s pair. But as her case shows, even without complications, AF is uncomfortable and requires treatment if it doesn’t disappear on its own.
“Although having a benign course, regular follow-up of patients with lone AF is warranted,” a group of Dutch researchers led by Dr. Bas Schoonderwoerd wrote in a 2008 paper. “In time, risk factors such as hypertension, heart failure, diabetes, and peripheral vascular disease may develop, changing prognosis.”
A separate trio of Dutch scientists followed a cohort of endurance athletes for ten years, and in a 2004 paper noted that AF developed in to permanent, chronic AF in fifteen percent of the study subjects.
Athletes should also be concerned about AF because it means that the heart is not pumping blood efficiently. Instead of producing one big electrical signal, the pacemaker cells in the atria beat chaotically, producing a group of weaker electrical signals. As a result, the atria pumps quickly; however, not all of these signals reach the ventricles, so they pump more slowly. The end result is that pumping is not as powerful.
So What’s the Big Deal?
“The absolute incidence of death during or within one hour of sports participation among U.S. high school and college athletes is one death per year for every 133,000 men and 769,000 women,” Dr. Thompson wrote in his 2002 paper. “These numbers overestimate the incidence of cardiac events, because of the 136 deaths, only 100 were caused by cardiac disease.”
An individual skier who shows signs of bradycardia or atrial defibrillation has only a miniscule chance of dropping dead on the trails; if their heart is otherwise healthy, the arrhythmias found by the Swedish researchers aren’t necessarily dangerous.
The more important finding of their study on the Vasaloppet skiers, however, was that as skiers trained and raced more and more, they because more likely to develop arrhythmias.
This concept is supported by previous research showing that there is some threshold of lifetime training volume above which arrhythmias become markedly more common. As athletes move into middle age and keep training, they are more likely to experience AF, and as they continue to age, they show more risk factors for serious complications – although even these complications are not as prevalent or as dangerous as some of the other heart problems which are common in the rest of the population.
In short, the more a skier trains, the more the heart restructures itself to deal with the stress of exercise – for better or for worse.
“The veteran athlete may not be as healthy as believed with many established areas lacking conclusive evidence to support the benefits of a lifelong career in high intensive endurance exercise,” a team of international researchers noted in a paper just last year.
While it’s not a reason to stop training, skiers should be cautious about heart health. It’s often difficult to tell whether abnormalities are due to athlete’s heart or an underlying condition, but if a skier is blacking out on the trails or experiences heart palpitations, they need to head to the doctor’s office – pushing so hard you see stars might actually be a serious condition.
Journal Sources
Hoogsteen J, Schep G, van Hemel NM, van der Wall EE. Paroxysmal atrial fibrillation in male endurance athletes: a 9 year follow up. Europace 2004;6(3):222-228.
Karjalainen J, Kujala UM, Kaprio J, Sarna S, Viitasalo M. Lone atrial fibrillation in vigorously exercising middle-aged men: a case-control study. British Medical Journal 1998;316:1784.
Mangrum JM, DiMarco JP. The Evaluation and Management of bradycardia. New England Journal of Medicine 200;342(10)703-709.
Partarrieu J. “Link Between Elite Cross-Country Skiing And Increased Risk Of Subsequent Arrhythmias“. Medical News Today, August 31, 2011. Web. 10 Sep, 2011.
Schoonderwoerd BA, Smit MD, Pen L, Van Gelder IC. New risk factors for atrial fibrillation: causes of ‘not-so-lone atrial fibrillation.’ Europace 2008:10(6):668-673.
Swanson DR. Atrial fibrillation in athletes: implicit literature-based connections suggest that overtraining and subsequent inflammation may be a contributory mechanism. Medical hypotheses 2006:66(6)1085-1092.
Thompson P. Exercise and the Heart: The Good, the Bad, and the Ugly. Dialogues in Cardiovascular Medicine 2002;7:143-162.
Viitasalo MT, Kala R, Eisalo A. Ambulatory electrocardiographic recording in endurance athletes. British Heart Journal 1982;47:213-220.
Wilson M, O’Hanlon R, Basavarajaiah S, George K, Green D, Ainslie P, Sharma S, Prasad S, Murrell C, Thijssen D, Nevill A, Whyte G. Cardiovascular function and the veteran athlete. European Journal of Applied Physiology 2010;3:459-478.




14 comments
campirecord
September 12, 2011 at 12:53 pm
1- First, and sadly, these findings have yet to make their way into any peered review paper, no Medical News Today isn’t one reference of any worth and maybe the index number on some of these other articles isn’t worth getting into.
2- Including and describing a cohort size as ELITE while at 160% of the winning time is questionnable.
3- Within that population, the largest difference was within the younger athletes, mostly for atrial fibrillation and bradyarrhythmias, which are considered a lot less serious than the “potentially lethal” ventricular arrhythmias. As you eloquently pointed out, I find this to be missleading of the title. The original data stemed articles and press release that show titles that are missleading and this is only a sign of modern media gone wrong.
4-There is absolutely no numbers against a normal sedentary population. Many people believe high intesity athletes may have more incidence of bradycardia as they push the machine, anyone ever had that good old throw up feeling… bradychardia can totally screw the numbers.
5-The press release skips some relevant details. It’s like the well-known trade-off for exercise of any sort: your chance of a heart attack rises temporarily during extreme exertion, but your overall odds of heart attack decline with exercise. In this case, it’s worth bearing in mind the findings from previous studies of the same race: the more Vasaloppets you do, the longer you live. So whatever the downsides of arrhythmias, they’re evidently outweighed by other benefits.
6-the more Vasaloppets you do, the longer you live. Yes, it is a Osteo paper yet the numbers clearly show, elite athletes who do the Vassalopet live longer.
Risk of Severe Knee and Hip Osteoarthritis in Relation to Level of Physical Exercise: A Prospective Cohort Study of Long-Distance Skiers in Sweden
http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0018339
7- this scientist seems to be having fun witha unique Vassalopet cohort data. Scientifically, it makes sense to push this unique data in as many possible papers, conference and press releases as possible. It is, after all, part of the publish or perish ridiculous culture.
Chelsea Little
September 12, 2011 at 6:57 pm
Campirecord:
While the Vasaloppet study has not yet been published and is not peer-reviewed at this point, the other papers are certainly legitimate. The British Medical Journal and the New England Journal of Medicine are two of the most respected medical journals out there. One of the papers I referenced has been cited over a hundred times in other peer-reviewed journal articles. While better research can always be done, the body of work on this subject is far from frivolous.
It will be interesting to see when the Swedish research team does write up their findings, and what conclusions they draw.
The osteoarthritis article you cite as being more reliable is using the same dataset – Vasaloppet participants from 1989 to 1998. It uses the same methodology, including the 160% classification, and in fact the paper has several of the same authors as the heart study.
highstream
September 12, 2011 at 11:44 pm
“but if a skier is blacking out on the trails or experiences heart palpitations, they need to head to the doctor’s office.”
All this for a conclusion that applies to anyone, skier or couch potato?
Chelsea, this article provides useful information for skiers. It’s just couched, including the title, in a way that comes across more sensationalistic than any data in it supports. Even at the extremes, there are Jim Fixx’s in skiing, just as there are in other parts of life. So what?
nexer
September 13, 2011 at 7:06 am
It’s not that people who do more Vasaloppets live longer, it’s that people who live longer do more Vasaloppets.
Bradycardia is only fatal when your HR gets to zero.
imnxcguy
September 13, 2011 at 10:23 am
Chelsea,
Thanks for reviewing this article. The more info about this out there, the better. As a 55 year-old lifetime XC ski racer, I’ve been dealing with my own personal bout of heart issues, including an enlarged heart wall and T-wave aberrations, as well as abnormally high blood pressure at extreme exertion. But “except” for these conditions, there are no other indications of heart disease or problems.
What I’ve found, however, is that while there are lots of these “studies” done, there’s not much help in the way of what to DO about these issues. I’ve been put on beta blockers (after little results with calcium channel blockers), and I hate being on them. But the risk-reward benefit is supposedly the important aspect, and without any solid information out there on this condition, you have to just go with what the doctors recommend, it seems. I’m waiting for the study that says, “Yeah, you got a weird heart. No worries, mate, carry on.”
The only positive aspect of all these tests is that they have proved that I do actually HAVE a heart, something that was contested for many years by friends and colleagues.
Mark Nadell
haltvick
September 13, 2011 at 11:39 am
There has been several heart issues among pro triathletes, in particular the athletes focusing on Ironman length races.
Steve Larson died of a heart attack while running intervals on a track. NORBA mtb National champion, Motorlola Pro Cycling Team member, Ironman Lake Placid champ. Age 39
Greg Welch had several bouts of his heart racing up to over 300 beats a minute during the 98′ Hawaii Ironman swim. Unwisely he finished the race, with several more incidents during the event.
After medical tests, he was diagnosed with ventricular tachycardia. If I remember correctly, he had to have a pace maker installed and forced to retire from sports, while in his 30’s.
With over 100 pro victories, including Hawaii Ironman World Championship and ITU World Championship.
In 2004, Australian ITU World champion Emma Carney retired from competition after her V-tach diagnosis. She was fitted with a defibrillator to stabilize her condition and has slowly made her way back into the sport, though she will never compete at the highest levels of the sport again.
Torbjørn Sindballe, Hawaii Ironman 3rd overall was forced to retire in 2009 with what is called a bicuspid aortic valve.
Norman Stadler, who won the Ironman World Champions in 2004 and 2006, had emergency heart surgery this summer to repair a failing heart valve and a nearby aortic aneurysm. He is 38 years old.
Other top professionals, like Ironman champ Scott Tinley and 2 time Ironman champ Peter Reid retired with destroyed immune systems.
Is it fair to compare the health problems of Pro Triathletes doing races that take 8+ hours to Pro XC ski racers racing for 1 or 2 hours? Maybe not. But I’d guess the overall training hours and race effort of someone like Petter Northug or Marit Bjorgen is similar to athletes in other endurance sports such as triathlons.
I’m not a doctor, scientist or elite athlete. But I have trained ‘hard’ and raced moto-cross, triathlons and XC ski races for 38 years, just like the life long endurance pro triathletes with heart issues.
Should I be worried about the 400 hours a year I put on my body compared to the athletes doing 800-1200 hours? When does training and racing turn from making us healthy, to ruining ourselves?
Are there any examples in XC skiing of top level competitors who have developed health issues? Or do all of them live to be 100 years old and still going strong? Chelsea has written a good article and I hope to learn more.
Paul Haltvick
campirecord
September 13, 2011 at 1:33 pm
People, I am all for talking about hearth issues for a few exceptions but the reality is that the USA is dying of fatness and coach potatoness, I don’t think I have to tell you how crippled this country will become soon. You are now an exception if your body index is normal, hearth failure, HBP and diabetes is rampant and cross country skiing will not add to this pandemia… Supersize me.
I also think there needs to be proper studies made on recovery and low level training. All this is fun but if were a fat pig watching a Vasslopet on TV with a burger in one hand and a coke in the other, I would think to myself ”this shit going to kill them kids !” cause I read it on the news.
Trollhaugen
September 14, 2011 at 9:45 am
Chelsea has written a very well-balanced and thoughtful article, and I was surprised by its quality. Surprised not because I doubt Chelsea’s ability as a writer, but as a physician I cringe when I see health-related stories written by (presumably) non medical professionals. Her headline was very accurate and in no way is fear-mongering or yellow journalism. I agree with campierecord that the population of this country (USA) is suffering an epidemic of obesity and its associated morbid conditions, but this story is in no way going to scare people off the trail and onto the couch. I thnk your criticism is unfair.
The issue of atrial fibrillation and atrial flutter occurring with higher prevalence in endurance athletes is well known and documented in many peer-reviewed journals such as European Heart Journal, Europace (European Society of Cardiology), Journal of the American College of Cardiology, Cardiology, American Journal of Physiology, Circulation, British Journal of Sports Medicine, and others, in addition to the ones cited in this article.
One of the premier electrophysiologists (cardiologist) in the world (Brugada. Check out “Brugada syndrome”) has published several articles on this. What is not definitively known are all the precise factors which cause this to happen. As with all research, one has to make conclusions based on the data regardless of your presuppositions. One presupposition we all had was that lots of exercise is good for you no matter what your age or level of fitness. What the studies so far show is that: 1) Incidence of atrial fibrillation increases with age. 2) There are at least two “kinds” of atrial fibrillation which affect athletes, the one which is induced during periods of intense activity, and another which seems induced by slow heart rate (vagally mediated) and occurs often during sleep when the heart rate in aerobically trained individuals is very slow (bradycardia). These probably occur by two completely different mechanisms. 3) Other things being equal, an older athlete will have a higher likelihood of suffering atrial fibrillation than a younger athlete, AND the older athlete will have a higher likelihood of sufffering atrial fibrillation than an age-matched non-athlete. 4) Incidence of atrial fibrillation increases with a lifetime training load of >1500 hours. This is not a hard number, like all of a sudden when the warranty runs out on your car things go wrong, but this has been found to be an important (yet not absolute,)threshold in the development of a-fib.
It is always difficult to wade through research articles and evaluate which ones are valid (study design, appropriateness of outcome measures, statistical considerations, etc) and many medical professionals aren’t even very good at it! Chelsea has done a good job and presented a very fair assessment of the body of knowledge on this subject as it exists at this time.
campirecord
September 15, 2011 at 1:53 pm
I absolutely agree that Chelsea did a great job with this press release. The reality, Trollhaugen, is that this article stems from major newswires from the Swedish lab after a meeting. Your typical ‘let’s get some crap on the news so we have something for the general public’. If you attend international meetings, you see that all the time.
It is true Chelsea nailed it, however, my review in the matter is mostly from what I have read every where else. Let’s take a look at what the sweds said in their press release from the european society of cardiology.
”Compared to those who had completed one single race, those who had completed 7 or more races had 29% higher risk of a subsequent arrhythmia. Further, elite athletes finishing at 100-160% of the winning time had 37% higher risk of arrhythmias than recreational athletes finishing at more than 241% of the winning time.”
In my mind, although there is something, this is truly a broad classification. I don’t have the number of folks who did their first Vassa at 100% of the winning time. I also do not know the fitness of an ELITE athlete who finishes at 160%. Actually, we have no absolute numbers. Also, the actual data suggests that the biggest difference where EXCLUSIVELY associated with FIB and BRADY. Considered a lot less serious than ventricular arrhythmia.
Also, Traullhaugen, I would like to submit that their numbers seem to go against the general consensus of the studies you have mentioned. Andersen’s presentation says: ”This association was more prominent among younger (less than 45 years) than older athletes. The associations were mainly driven by the most common type of arrhythmia, atrial fibrillation, and bradyarrhythmias. We did not find any significantly increased incidence of the potential lethal ventricular arrhythmias with any of the exposures. ”
Dr. Andersen summarizes: “Basically, this study shows, that even though physical activity is generally healthy, athletes committed to endurance sports at elite level have higher risk of suffering from a heart rhythm disorder… We emphasize that we do not find any increased incidence of potential lethal heart rhythm disorders. However, this study only compares athletes at different levels and a future large scale study comparing athletes against the normal population would be very interesting.”
???
Frankly, I truly think a Vassa will not change my risk-benefit assessment compared to general population.
Finally, I would like to add this. I had a chance to consult one of the two Brugada’s as a genetic expert as he was in Montreal for a short term. I want to point out few things: 1-Brugada had set up a linkage lab because the Brugada Syndrome is a GENETIC disorder 2-There is some evidence out there that many athletes who overtrain also ‘overuse’ if you know what I mean, take it from a hockey dad… 3- It is ironic that Dr. Brugada was temporarily working in a research institute which no less than 2 weeks ago, had to fire one scientist for forging data in a minimum of two PNAS papers on miRNA gene expression in hearth failure, the scientist was photoshoping RNA blots at will for about 5 years before being caught.
My apologies for my cynicism, I have been around scientists for too long. My intent was certainly not to discredit Chelsea’s great article but I also know that it was the swedish study that most probably started this article. It is the study I question the most and by no means a large part of the summerised article from Chelsea.
This is because scientists now are pretty good at PR now. Chelsea, I am pretty sure you know that. The number of retraction have skyrocketed in the last decade:
http://www.guardian.co.uk/science/2011/sep/05/publish-perish-peer-review-science
If I had a dollar for every PR when a scholar found a new molecule against cancer, I’d be a millionnaire !
Call me the cloxxci of science…
skiheidi
September 16, 2011 at 6:32 am
Wow, I really had to search for my login info, have not logged in for a long time.
I am not sure what conclusions can really be drawn from this data. One thing to pay attention to is there is a difference between correlation and cause and effect.
There are so many things we do not know about hearts, and each person’s situation is different.
I have a situation where when I have a critical mass of negative physiological stress of certain kinds (overheating, dehydration, low blood sugar) my heart rate goes up really high, sometimes 240+ or maxing out the heart rate monitor. Overheating is the biggest factor. The first time it happened was when I was 11, and it has happened occasionally ever since, though less and less often over time and less and less extremely (not as high of heart rates, and they come down to normal more quickly) over time. (I have continued to exercise a lot aerobically, every year.) Intensity or duration of exercise don’t tend to cause it in any immediate sense, but if my ratio of intensity to aerobic exercise is too high for an extended time (like a couple of months) then it happens more easily. So it is important for me to maintain a good amount of aerobic, lower intensity exercise as I add intensity, not go too far into an extreme of cutting volume to accommodate intensity. It’s a balance. (I also tend to be faster and have better recovery, if I don’t cut the volume too extremely, which isn’t the “typical” way most athletes are, apparently.) The first doctor I saw about it said it was just a symptom of heat stroke and I should make sure I do not get overheated. But then it happened when I was swimming in cold water, so it was clear it was not just that. Another doctor said it was ventricular fibrillation, which is harmless, but I should avoid the stresses that cause it because it is a sign I am overstressed. He says that with fibrillation, atrial fibrillation is much more dangerous because it can cause a stroke by causing a blood clot to form. I had an electrocardiogram at one point, when I was 18, and my heart was completely normal, even though I had had a lot of these events in my teens. My mother, who, like me, has hypoglycemia, also, like me, sometimes has similar events of her heart going extremely fast. So it seems there is a genetic component and possibly a connection with hypoglycemia, which is one thing that can bring it on. Part of why I exercise so much is actually to manage my blood sugar, so there is a correlational factor involved in the connection to the fast heart rate, that is not cause and effect. I think the reasons I have had less and less of a problem are because I have paid attention to what causes it and changed things around in order not to cause it, with training, and also with nutrition and hydration strategies. With hydration, what works best for me is to get adequate balanced electrolytes with the hydration, particularly things OTHER THAN NaCl- that is, other than salt. This involves eating fruits and vegetables, and using health-f00d recovery drinks or making my own, that contain fruit juice and sources of magnesium (ex. algae). If I go on a trip and do not get an adequate intake of fruits and vegetables, even for a few days, my electrolyte balance gets pretty screwed up. Everyone needs to figure out their own best nutrition strategies by keeping track of what works and what does not. Nutrition is highly individual, so my advice about that is to pay attention to whether your nutrition is really working, and experiment. Also, anytime I have had an abnormally elevated heart rate, I have stopped as soon as possible (it’s OK to swim slowly to the edge of a lake if I’m in the middle- I don’t actually float, so I have to unless I have a spotter) and rest. And for the next 48 hours I go ahead and train, but nothing high stress- nothing really hard or really long. If I have more than one incident in a 3 month period, I also make a habit of napping. (Napping regularly has a huge healing effect that I do not completely understand. There is quite a bit of research showing napping to be great for heart health.) One time I was actually advised by an acupuncturist to do this- take a nap every day in the middle of the day. It’s hard to schedule but it is very effective at giving the body a chance to make needed neurological corrections, including heart rhythms. I think my practice of making recovery from it the top priority, anytime it has happened, as contributed to the reduction in frequency and extremity of the occurrences.
I am sharing this because it might help other athletes and it also demonstrates how individual this stuff is and how important it is to learn to listen to your body, not just read the scientific literature. A combination of listening to your body and reading scientific information (and not just about exercise physiology) is good, in my experience. Part of why I have been able to figure out what I have is also that I kept training logs starting when I was 14, with resting heart rates and all sorts of stuff- some information only becomes clear to me when I look that far back! Keep your training logs- they may reveal something to you years later.
One thing this also points to is that athletes need to respect each others’ individual physiological differences and what each person has figured out about their body. There isn’t a “right” way to train, or to eat, or to do pre-race recovery, or anything else. Athletes need to respect each other about each person’s unique body and what they have figured out about how to take care of themselves.
skiheidi
September 16, 2011 at 6:47 am
PS
Another thing that really helps is adequate cooldown, plus an easy recovery workout at a different time, after intensity, even if I feel “tired” (which I really think is partly psychological, especially after a race). I recover better, especially in my heart and other muscles, I feel better the next day, and my incidence of this fast heart rate happening on the day after a hard workout is much lower if I do this. When I was 14, I had a high incidence of the fast heart rate thing, as I called it then, on the day after a level 4 or 5 interval workout if it was my 2nd or 3rd intensity session of the week, and in the second of two back to back intensity workouts days. Almost 50%. And that was when most of these things occorred- in one of those two situations. With adequate cooldown and recovery workout following intensity, the incidence of fast heart rate events on the day after a hard workout or on the second day of back to back intensity workouts is close to zero. Getting adequate cooldown and recovery distance has almost completely eliminated that particular pattern. So now, when I say that intensity in itself, in the short term, does not especially bring it on, that fact is a result of my having found a way to make that the case! At present, overheating is really the main culprit I still need to watch out for. Most other causes, I have effective strategies for preventing and they rarely come up. And the overall incidence of this has gone down to 1-2 times per year, whereas when I was 14 it was not unusual to have it happen twice or more in one week.
skiheidi
September 16, 2011 at 7:00 am
I should add that the first time I had this happen was not in a sports situation but in preparation for a junior high marching band performance, standing around in a hot parking lot, wearing a costume that was too hot. I wasn’t exercising and wasn’t dehydrated. I could have been hypoglycemic- it was before I had much awareness of that. I was definitely overheated.
skiheidi
September 16, 2011 at 7:10 am
In the article, “inflammation caused by training,” as a possible cause, sticks out to me. Inflammation levels are not just determined by what you do for training!! There are other factors, some of which we might not even be aware of. A good cooldown and recovery workout after intensity really helps; so does good nutrition. A diet high in simple carbs tends to encourage inflammation. A diet high in vegetables tends to decrease inflammation. So a diet of packing in the calories via simple carbs, sugars, white rice, white flour, etc, has its drawbacks. Balance. Some simple carbs at certain times are OK, but if it gets to be your entire diet, your inflammation level will go up. Eat the powerbar (if you are going to eat simple carbs, those are a good choice because they have some other nutrition too) after the workout, but have a nutritious dinner, something like that. Hydration also helps a lot.
Keeping inflammation levels down is important for A LOT of reasons, including, also, there is an elevated tendency for endurance athletes to get deep vein thrombosis, especially when traveling long distances in vehicles, and keeping inflammation levels in check helps with that.
That’s all for now….sorry to write so much, but I am trusting that people who don’t want to read it, won’t, and it might help someone, so I wrote it. Have a good day.
Tim Kelley
June 14, 2013 at 11:11 am
I didn’t read the article, went straight to the comments. Great, informative comments. Right on Campi!